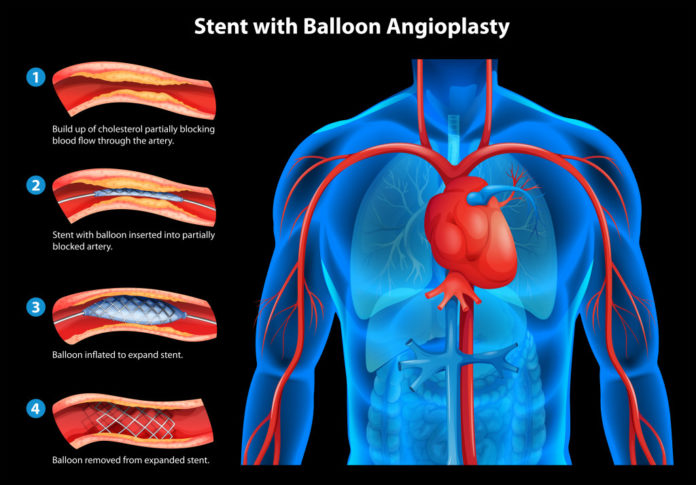
Placing a stent in the heart vessels aims at expanding narrowed coronary vessels. With these, thrombosis or ruptured atherosclerotic plaques, if any, are blocked. Stanning is a method of behavior in emergency situations and, in a large percentage, are life-saving when developing a myocardial infarction. They are also planted after significant coronary defects have been detected by coronarography.
Place as many stents as it is deemed necessary. There is an explanatory sense of reassurance, given the good prognosis that theoretically (and actually) follows. However, it is appropriate to know a detail that seems at first glance unexpected. And this is that this stent may become clogged and follow the same complications as in the initial thrombosis. The condition is called stent-thrombosis and it is good to know both doctors and patients.
Stent thrombosis is a complication that occurs in 1-2% of patients.
If not recognized on time, it can cause serious health damage, myocardial infarction and poor outcome. It is due to clogging with a clot of a stent placed in the coronary vessels. Even if it can not be proven, retrofit can be thought of in the development of a myocardial infarction in the stent area as well as any unexpected death within one month of manipulation.
Stent-thromboses are divided into three main types according to the moment of occurrence. When it happens in less than a month we talk about early retrombosis. It, in turn, is acute if it is less than a day after the procedure. Late is in the month to one year range and is very late if it is more than a year late.
What are the factors that predict them?
Some patients have insensitivity to the ongoing dual anti-inflammatory therapy, which holds the blood one degree more diluted than normal. Others do not interrupt or inadvertently intake these medications. As a body alien to the body, stent automatically increases the risk of clotting afterwards. Diabetes mellitus and renal insufficiency to a great extent also increase the risk of stent-thrombosis. The factors associated with the stent itself are determined by its shape, material, size, and so on.
The third group of factors causing an increased risk of retrothrobes are those associated with the procedure. After stenting, local blood flow in the coronaries changes, which in turn leads to increased clotting. It is also possible to break the wall of the container during manipulation. Not without meaningful how many stents are common, when placed, and so on.
What is being done to reduce this risk?
By default, post-treatment for about one year is anti-aggregation therapy, which may vary according to some additional factors. It is the twelve-month limit where it reduces the high risk of retromobia and avoids the inevitable risk of bleeding. It is well-known, in the case of a drug disorder of blood clotting, the likelihood of uncontrollable or massive bleeding greatly increases.
But what else is widely used today? These are the drug-emitting stents. Their special structure contains a substance that would otherwise have to be taken as a daily tablet formulation. By acting locally at the site of the stent itself, medications greatly reduce the likelihood of retrothrobes. Then the risk period after the procedure can be reduced even in half.
Why, when and if retromoblasts appear at all is something that can not be fully predicted. However, this does not reduce the immense benefit of stenting. Neither should dissuade someone from the procedure. However, caution is required to avoid myocardial infarction, although at some point a stent has already been placed in a particular coronary artery.